In this section of our NREMT Study Guide, we will help you prepare for the airway, respiration, and ventilation portions of the EMT exam. It’s around 18–22% of the exam.
This section of our study guide cover the anatomy of the respiratory system, the physiology of breathing, airway management, oxygen therapy, opening a patient’s airway using different maneuvers, airway adjuncts used by EMTs, and oxygen-delivery equipment.
After you have reviewed this section of the study guide, there will be practice questions to test your knowledge of the material.
You can also download the complete study guide PDF for free.
Anatomy of the Airway
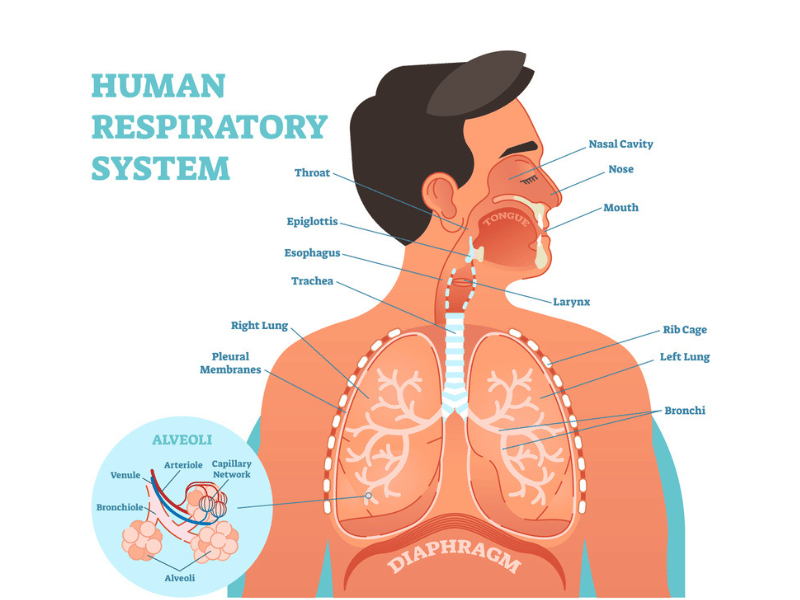
The airway is the path that air follows from the atmosphere to the alveoli. It is divided into the upper and lower airways.
The Upper Airway
The upper airway’s function is to warm, filter, and humidify inhaled air. It consists of all structures above the vocal cords.
- Nose and Mouth: The entry points for air. The nasal cavity is called the nasopharynx, and the oral cavity is the oropharynx.
- Pharynx: The throat; a muscular tube that serves as a common passageway for air and food. It extends from the back of the nose and mouth down to the esophagus and larynx.
- Larynx: The voice box; a cartilaginous structure that marks the end of the upper airway. It contains the vocal cords.
- Epiglottis: A leaf-shaped flap of cartilage at the base of the tongue that covers the opening of the larynx during swallowing to prevent food and liquid from entering the trachea.
- Cricoid Cartilage: A firm, complete ring of cartilage that forms the lowest portion of the larynx. It is the only complete cartilaginous ring in the upper airway.
The Lower Airway
The lower airway’s sole function is to conduct air to the site of gas exchange. It begins below the larynx.
- Trachea: The windpipe; a tube that extends from the larynx into the chest, held open by C-shaped cartilage rings.
- Carina: The point at which the trachea divides into the right and left mainstem bronchi.
- Bronchi and Bronchioles: The mainstem bronchi enter each lung and continue to branch into smaller and smaller tubes. The smallest of these are the bronchioles.
- Alveoli: Microscopic air sacs at the end of the bronchioles. The alveoli are the functional units of the lungs where gas exchange occurs. They are encased in a network of pulmonary capillaries.
Opening a Patient’s Airway
Ensuring a patent airway is the first priority in patient care. In an unresponsive patient, the tongue is the most common cause of airway obstruction.
Your initial assessment determines the priority.
- ABC (Airway, Breathing, Circulation): Used for most patients.
- CAB (Circulation, Airway, Breathing): Used for patients with obvious signs of life-threatening external hemorrhage. Bleeding control is the priority.
Opening and Clearing the Airway
Positioning for Airway Management:
- Sniffing Position: The optimal position for maintaining a patent airway and for ventilation. The head and chin are thrust slightly forward. For a supine patient, this can be achieved by placing a small towel under the patient’s shoulders and back, which helps keep the trachea straight and aligned.
Manual Airway Maneuvers:
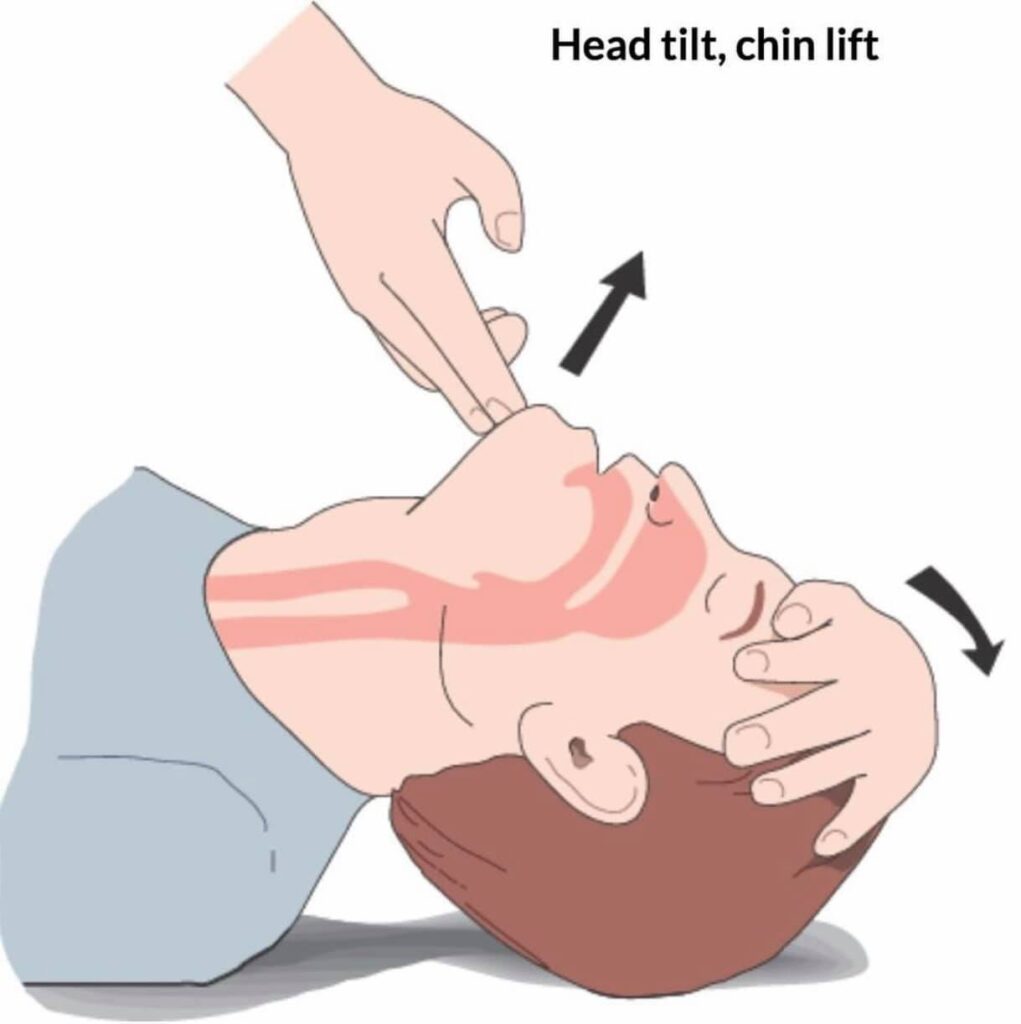
- Head Tilt-Chin Lift: The primary method for opening the airway in a non-trauma patient. Place the heel of one hand on the patient’s forehead and apply firm pressure to tilt the head back. Place the fingertips of your other hand under the bony part of the lower jaw and lift the chin upward.
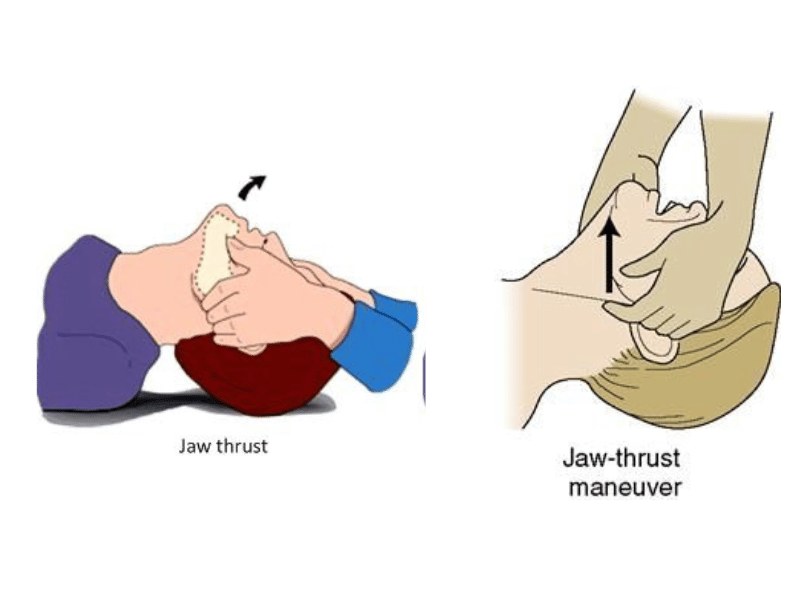
- Jaw-Thrust Maneuver: The preferred method if a cervical/spinal injury is suspected. Kneel above the patient’s head, place your fingers behind the angles of the lower jaw, and move the jaw upward with your index and middle fingers while your thumbs help position the jaw. This maneuver is performed without tilting or extending the head. Important: If the jaw-thrust maneuver fails to open the airway, the head tilt-chin lift must be used as a last resort, as a patent airway is the immediate priority.
Foreign Body Airway Obstruction (FBAO):
- Mild/Partial Obstruction: The patient can still speak, cough, and breathe. Wheezing or stridor may be present. Encourage the patient to cough forcefully. Provide oxygen, place them in a position of comfort, and transport rapidly. Do not perform abdominal thrusts.
- Severe/Complete Obstruction: The patient cannot speak, breathe, or cough effectively. They may clutch their throat (the universal sign for choking).
- Conscious Adult/Child: Perform abdominal thrusts (Heimlich maneuver). Stand behind the patient, make a fist, and place the thumb side against the patient’s abdomen just above the umbilicus and below the xiphoid process. Press into the abdomen with quick, inward and upward thrusts.
- Conscious Pregnant/Obese Patient: Perform chest thrusts in the same location as chest compressions.
- Conscious Infant (Under 1 Year): Perform 5 back blows between the shoulder blades with the heel of your hand, followed by 5 chest thrusts on the lower part of the sternum with two fingers.
- If Patient Becomes Unresponsive: Immediately begin CPR, starting with chest compressions. Before attempting ventilations, look inside the mouth for the object and remove it with a gloved finger only if it is visible.
Suctioning:
Suctioning is used to remove fluids like blood, vomit, or secretions from the airway. A suction unit should generate a vacuum of at least 300 mmHg.
- Catheters:
- Rigid (Yankauer/Tonsil-tip): Best for suctioning the oropharynx. Its large diameter will not easily collapse.
- Flexible (French/Whistle-tip): Used for suctioning the nose, a stoma, or when the patient’s teeth are clenched.
- Technique:
- Assemble the unit and test for adequate vacuum pressure.
- Measure the catheter from the corner of the patient’s mouth to the earlobe.
- Turn the patient’s head to the side (if no c-spine injury).
- Open the mouth and insert the catheter only as far as you can visualize (to the depth measured).
- Apply suction in a circular motion only while withdrawing the catheter.
- Crucial Time Limits: Suction for no longer than 15 seconds in an adult, 10 seconds in a child, and 5 seconds in an infant. Prolonged suctioning causes hypoxia and can stimulate the vagus nerve, leading to severe bradycardia.
Assessment of Breathing
Assessing Breathing
Normal Respiratory Rates by Age:
- Adult (18+ years): 12 to 20 breaths/minute
- Adolescent (13-18 years): 12 to 16 breaths/minute
- School-Aged (6-12 years): 18 to 30 breaths/minute
- Preschooler (4-5 years): 22 to 34 breaths/minute
- Toddler (1-3 years): 24 to 40 breaths/minute
- Infant (0-12 months): 30 to 60 breaths/minute
Signs of Inadequate Breathing (Respiratory Distress/Failure):
- Rate: Too fast (tachypnea) or too slow (bradypnea) for the patient’s age.
- Rhythm: Irregular breathing pattern.
- Quality: Diminished, noisy, or absent breath sounds. Unequal or shallow chest expansion.
- Effort: Use of accessory muscles in the neck, abdomen, or between the ribs (retractions). Nasal flaring, especially in children. Tripod positioning.
- Skin: Cyanosis (bluish discoloration), pale, or cool, moist skin.
Signs of Inadequate Oxygenation (Hypoxia):
- Early Signs: Restlessness, irritability, apprehension, anxiety, tachycardia (fast heart rate), and tachypnea.
- Late Signs: Altered mental status, confusion, lethargy, weak/thready pulse, cyanosis, bradycardia (slow heart rate, especially in children), and bradypnea.
Pulse Oximetry (SpO2):
A pulse oximeter measures the percentage of hemoglobin that is saturated with oxygen. It is a valuable tool but has significant limitations:
- Inaccurate Readings: Caused by dark/metallic nail polish, dirty fingers, poor perfusion (hypovolemia, shock), severe peripheral vasoconstriction (hypothermia, smoking), or bright ambient light.
- Carbon Monoxide (CO) Poisoning: This is the most critical limitation. The pulse oximeter cannot differentiate between oxygen and carbon monoxide bound to hemoglobin. A patient with severe CO poisoning will have a falsely high SpO2 reading (e.g., 100%) despite being critically hypoxic.
Lung Sounds (Auscultation):
- Stridor: A high-pitched, brassy, crowing sound heard primarily on inhalation. Indicates a partial upper airway obstruction (e.g., foreign body, croup, epiglottitis).
- Wheezing: A high-pitched whistling sound, most prominent on exhalation. Caused by constriction of the lower airways (bronchioles). Common in asthma, COPD, and anaphylaxis.
- Rhonchi: Low-pitched, noisy, rattling sounds, like snoring or rumbling. Prominent on exhalation. Suggests mucus or fluid in the larger airways. Common in bronchitis and pneumonia.
- Crackles (Rales): Wet, popping, or crackling sounds, like cellophane being crumpled. Heard on inspiration. Caused by air passing through fluid in the alveoli. The classic sound of pulmonary edema (CHF) or pneumonia.
- Gurgling: Sound of fluid in the upper airway; requires immediate suctioning.
- Snoring: Sound of the tongue partially obstructing the upper airway.
- Vesicular: Normal, clear breath sounds.
Interventions & Equipment
Airway Adjuncts
Airway adjuncts are used to maintain a patent airway in unresponsive or semiconscious patients. They do not protect against aspiration.
- Oropharyngeal Airway (OPA): A curved plastic device that holds the tongue off the posterior pharynx.
- Indications: Unresponsive patients without a gag reflex.
- Contraindications: Conscious patients or any patient with an intact gag reflex. Also contraindicated for caustic substance ingestion.
- Sizing: Measure from the corner of the patient’s mouth to the earlobe.
- Insertion: Insert the OPA with the tip pointing toward the roof of the mouth. Advance until you feel the soft palate, then rotate it 180° into place. For children, use a tongue depressor to hold the tongue down and insert the OPA directly without rotation.
- Nasopharyngeal Airway (NPA): A soft, flexible tube inserted through a nostril into the posterior pharynx.
- Indications: Semiconscious or unconscious patients with an intact gag reflex who will not tolerate an OPA.
- Contraindications: Severe head injury with blood draining from the nose or a history of a fractured nasal bone. Suspect a basilar skull fracture if you see cerebrospinal fluid (CSF) draining from the ears, ecchymosis under the eyes (raccoon eyes), or behind one ear (Battle’s sign).
- Sizing: Measure from the tip of the patient’s nose to the earlobe.
- Insertion: Lubricate the airway well. Insert into the larger nostril with the bevel facing the septum.
Oxygen Delivery
Oxygen Cylinders:
- Always “crack” the cylinder (briefly open the valve) before attaching the regulator to remove dust.
- A full cylinder contains approximately 2,000 psi.
- Common Sizes and Constants (for calculating duration):
- D Cylinder: 350 L (Constant: 0.16)
- E Cylinder: 625 L (Constant: 0.28)
- M Cylinder: 3,000 L (Constant: 1.56)
- G Cylinder: 5,300 L (Constant: 2.41)
- H/K Cylinder: 6,900 L (Constant: 3.14)
Oxygen Delivery Devices:
- Nasal Cannula (NC):
- Flow Rate: 1–6 L/min
- O2 Concentration: 24–44%
- Use: For patients with mild hypoxia who cannot tolerate a mask (e.g., COPD patients, claustrophobia). Not appropriate for patients in significant distress.
- Non-Rebreather Mask (NRB):
- Flow Rate: 10–15 L/min
- O2 Concentration: Up to 90-95%
- Use: The preferred device for patients with adequate breathing who are hypoxic and require high-flow oxygen.
- Key Point: Always fill the reservoir bag with oxygen before placing the mask on the patient.
- Bag-Valve Mask (BVM):
- Flow Rate: 15 L/min
- O2 Concentration: Nearly 100% with a filled reservoir bag.
- Use: For patients in respiratory arrest or with inadequate breathing (respiratory failure).
- Ventilation Rates: 1 breath every 6 seconds for adults; 1 breath every 2-3 seconds for children/infants.
- Technique: Deliver each breath over 1 second, just enough to produce visible chest rise. The two-person technique is far superior for maintaining a good mask seal.
- Common Complications: Poor mask seal, incorrect head position, gastric distention (from ventilating too fast or too forcefully), barotrauma (lung injury from pressure), and decreased cardiac output from increased intrathoracic pressure.
- Mouth-to-Mask (Pocket Mask):
- O2 Concentration: About 55% when supplemental oxygen is attached at 15 L/min. A one-way valve prevents backflow of secretions.
- Continuous Positive Airway Pressure (CPAP):
- Function: A non-invasive device that provides continuous pressure to keep alveoli from collapsing, pushing fluid out of the alveoli and improving gas exchange.
- Indications: Alert patients in moderate to severe respiratory distress from conditions like pulmonary edema or COPD, with a rapid breathing rate (>26/min) and low pulse oximetry (<90%).
- Contraindications: Respiratory arrest, hypoventilation, hypotension (systolic BP < 90 mmHg), chest trauma/pneumothorax, active GI bleed or vomiting, or inability to tolerate the mask.
- Complications: Claustrophobia, gastric distention, and hypotension due to decreased blood return to the heart.
- Venturi Mask: Delivers precise, low-to-moderate oxygen concentrations (e.g., 24%, 28%, 35%, 40%) based on the selected adapter.
Advanced Airways (EMT Awareness)
While EMTs do not typically place these, you must be able to assist and recognize them.
- Supraglottic Airway (e.g., King LT, i-gel): An airway device that sits above the glottis. It is indicated for failed endotracheal intubation. Placement is confirmed by bilateral breath sounds and an end-tidal CO2 detector.
- Endotracheal Intubation: The placement of a tube directly into the trachea. The mnemonic BE MAGIC outlines the steps for a provider: Bag-valve mask pre-oxygenation, Evaluate airway, Manipulate patient, Attempt intubation, GI (use supraglottic if unable), Intubation, Confirm placement.
- Tracheostomy Tube (e.g., Shiley): A tube placed in a surgical opening (stoma) in the neck for long-term airway management. These patients may require suctioning directly through the tube.
Pathophysiology of Respiratory Emergencies
Obstructive Diseases:
- Asthma: Chronic disease with acute exacerbations of bronchoconstriction, inflammation, and mucus production. Presents with wheezing, dyspnea, and anxiety.
- COPD (Chronic Obstructive Pulmonary Disease): A slow, progressive disease, most often caused by smoking.
- Chronic Bronchitis: Inflammation of the bronchioles and excessive mucus production, leading to a productive cough and rhonchi (“wet lungs”).
- Emphysema: Destruction of the alveoli, which leads to trapping of stale air. Causes an unproductive cough, barrel chest, pursed-lip breathing, and wheezing (“dry lungs”).
- Anaphylaxis: A severe, systemic allergic reaction that can cause rapid swelling of the upper airway (angioedema) and bronchoconstriction, leading to stridor and wheezing.
Fluid-Related Emergencies:
- Acute Pulmonary Edema: Fluid builds up inside the alveoli, impairing gas exchange. Usually a result of congestive heart failure (CHF). Presents with severe dyspnea (especially when lying flat), crackles (rales), and sometimes pink, frothy sputum.
- Pleural Effusion: A collection of fluid in the pleural space, outside the lung. It compresses the lung and causes dyspnea.
Infectious Diseases:
- Pneumonia: An infection of the lung tissue that causes inflammation and fluid buildup in the alveoli. Presents with fever, chills, a productive cough, and localized crackles or rhonchi.
- Epiglottitis: A life-threatening bacterial infection causing severe inflammation of the epiglottis. Classic signs are high fever, sore throat, drooling, and stridor.
- Croup: A viral infection of the upper airway in children, characterized by a low-grade fever and a “seal-bark” cough and stridor. Humidified oxygen may be indicated for extended transport.
Vascular and Traumatic Emergencies:
- Pulmonary Embolism (PE): A blood clot (or air bubble/foreign body) that lodges in the pulmonary arteries, blocking blood flow to a portion of the lung. Presents with a sudden onset of dyspnea, sharp chest pain, and tachycardia.
- Pneumothorax: Air in the pleural space, causing the lung to collapse.
- Spontaneous Pneumothorax: Occurs without trauma, common in tall, thin men. Presents with sudden dyspnea and pleuritic chest pain.
- Open Pneumothorax: An unsealed opening in the chest wall allows air to enter the pleural space.
- Tension Pneumothorax: A life-threatening emergency where air enters the pleural space but cannot exit. Pressure builds, collapsing the lung and shifting the heart and great vessels (mediastinal shift), which leads to obstructive shock. Signs include severe respiratory distress, absent lung sounds on the affected side, tracheal deviation (a late sign), JVD, and hypotension with narrowing pulse pressures.
- Hemopneumothorax: Blood and air in the pleural space.
Toxicological Emergencies:
- Carbon Monoxide (CO) Poisoning: CO is an odorless, colorless gas that displaces oxygen from hemoglobin. Presents with flu-like symptoms, headache, confusion, and syncope. Treatment is high-flow oxygen.
- Cyanide Poisoning: A rapidly acting poison that prevents cells from using oxygen. Presents with dyspnea, flushed skin, tachycardia, altered mental status, and seizures, leading to cardiac arrest.
Part 5: Special Populations & Considerations
Pediatric Patients
Children are not small adults. They have critical anatomical and physiological differences.
- Anatomy:
- Tongues are proportionally larger.
- Tracheas are smaller, softer, and more easily obstructed.
- The cricoid ring is the narrowest part of the airway in a young child.
- They are obligate nose breathers as infants.
- They rely heavily on their diaphragm for breathing (“belly breathers”).
- Assessment:
- Use the Pediatric Assessment Triangle (PAT): Appearance (muscle tone, interactiveness), Work of Breathing, and Circulation to the Skin.
- Signs of Increased Work of Breathing in Children:
- Nasal flaring
- Grunting (an attempt to create PEEP)
- Retractions (substernal, intercostal)
- Head bobbing
- Tachypnea
- Tripod position
- Key Physiological Point: Bradycardia in a child is a sign of critical hypoxia and imminent respiratory arrest. Children compensate for shock with tachycardia; hypotension is a very late and ominous sign. Capillary refill is a more reliable indicator of perfusion in children than blood pressure.
Other Important Concepts
- Gastric Distention: A common complication of BVM ventilation, especially in children. To alleviate it in a patient with a suspected spinal injury, use a spinal motion restriction device to carefully roll the patient to one side and apply firm but gentle pressure to the upper abdomen.
- Hyperventilation: Over-breathing that causes a drop in arterial CO2, leading to respiratory alkalosis. This can be caused by anxiety or a medical condition like diabetic ketoacidosis or an aspirin overdose. It results in dizziness, numbness/tingling, and muscle spasms in the hands and feet (carpopedal spasms).
- Body Temperature:
- Hyperthermia (Heat Stroke): Temperature >104°F.
- Hypothermia: Affects respiratory drive. At 92-89°F, respirations and pulse slow. Below 88°F, the patient may become unresponsive with very slow respirations.
- Burns: Airway compromise is a primary concern. Suspect airway burns if there are facial burns, singed nasal hairs, or soot in the mouth. These patients require high-flow oxygen and rapid transport, as swelling can rapidly obstruct the airway. Cover burns with a dry sterile dressing.
- Acidosis/Alkalosis: The respiratory system plays a key role in regulating the body’s pH balance. Acidosis is a buildup of acid (low pH), and alkalosis is a buildup of base (high pH). Conditions like DKA cause a metabolic acidosis, and the body compensates by breathing faster and deeper (Kussmaul respirations) to blow off CO2.
